5 Ways to Worsen Endometriosis
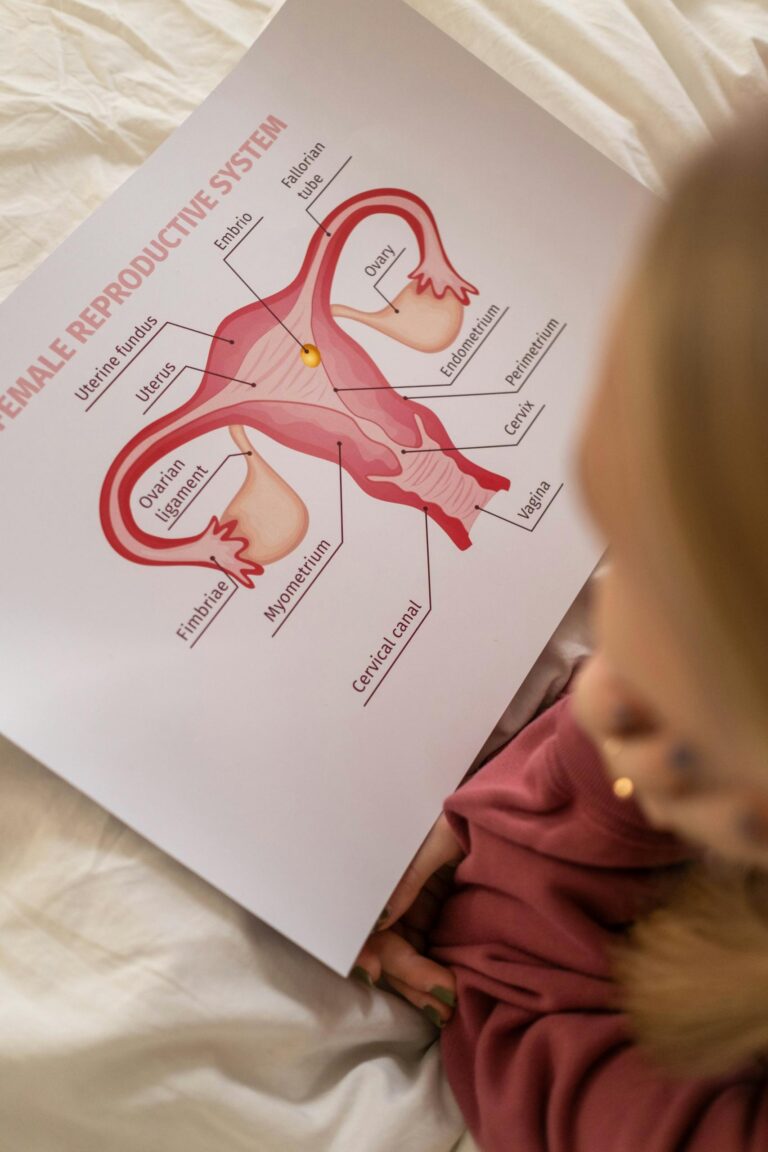
Endometriosis is a chronic condition where tissue similar to the uterine lining grows outside the uterus, causing pain, inflammation, and other symptoms. There are ways to worsen endometriosis without realizing it. While there’s no cure, certain factors can exacerbate the condition, worsening symptoms and making management more difficult. Here are five things that can make endometriosis worse, with explanations of why and strategies to mitigate their impact.
1. Chronic Inflammation
Inflammation plays a significant role in the development and progression of endometriosis. Consuming inflammatory foods, leading a sedentary lifestyle, or having untreated chronic conditions (such as diabetes and hypertension) can exacerbate inflammation, making endometriosis symptoms worse.
- Why it Worsens Endometriosis:
Inflammatory cytokines (chemical messengers of the immune system) are elevated in endometriosis patients, contributing to pain, swelling, and the growth of endometrial-like tissue. A diet high in refined sugars, trans fats, and processed foods promotes chronic inflammation, further exacerbating symptoms. - Examples of Inflammatory Triggers:
- Refined carbohydrates (white bread, pastries)
- Sugary beverages
- Fried foods and trans fats (e.g., fast food, margarine)
- Processed meats (e.g., bacon, sausages)
- What You Can Do:
- Adopt an anti-inflammatory diet rich in omega-3 fatty acids (found in salmon, walnuts, and flax seeds), colorful fruits and vegetables, whole grains, and lean proteins.
- Include herbs and spices with anti-inflammatory properties, like turmeric and ginger.
- Engage in regular moderate-intensity exercise to reduce systemic inflammation.
2. Hormonal Imbalance
Endometriosis is an estrogen-dependent condition. High levels of estrogen, relative to progesterone, can fuel the growth of endometriotic lesions, worsening pain and other symptoms.
- Why it Worsens Endometriosis:
Excess estrogen stimulates the growth of endometrial-like tissue. This imbalance can result from environmental factors (e.g., endocrine disruptors), obesity (which increases estrogen production in fat tissue), or inadequate liver detoxification (which can be negatively influenced by food intake). - Common Hormonal Disruptors:
- Plastics containing BPA and phthalates
- Non-organic animal products with added hormones
- Hormonal birth control that exacerbates estrogen dominance for some individuals
- What You Can Do:
- Work with a healthcare provider to assess and balance your hormone levels.
- Reduce exposure to endocrine-disrupting chemicals by avoiding plastic containers, canned foods with BPA linings, and conventional cleaning products.
- Support liver health with cruciferous vegetables (broccoli, Brussels sprouts, cauliflower, kale, arugula, etc.) and adequate hydration to help detoxify excess estrogen.
- Consider natural hormone-balancing interventions, like magnesium and B vitamins, under the guidance of a healthcare professional.
3. High Levels of Stress
Chronic stress worsens many chronic conditions, including endometriosis. Stress doesn’t cause the condition but can intensify symptoms like pain, fatigue, and hormonal fluctuations.
- Why it Worsens Endometriosis:
Stress triggers the release of cortisol, a hormone that can interfere with reproductive hormone balance. Additionally, stress can lead to heightened pain perception and exacerbate inflammation, creating a vicious cycle. - Signs of Stress Affecting Endometriosis:
- Increased frequency or severity of pelvic pain
- Worsening fatigue
- Difficulty sleeping or increased anxiety about symptoms
- What You Can Do:
- Incorporate stress-management techniques, such as mindfulness meditation, yoga, or deep breathing exercises.
- Schedule time for self-care activities you enjoy, like reading, crafting, or spending time in nature.
- Consider counseling or therapy to address the emotional impact of living with a chronic condition.
- Practice progressive muscle relaxation to ease tension and improve sleep quality.
4. Lack of Proper Nutrition
A nutrient-deficient diet can worsen symptoms by failing to provide the body with essential tools to combat inflammation, balance hormones, and repair damaged tissues.
- Why it Worsens Endometriosis:
Poor nutrition, particularly deficiencies in key nutrients like magnesium, zinc, vitamin D, and antioxidants, can leave the body less equipped to manage pain and inflammation. Diets high in simple sugars and processed foods can spike insulin levels, contributing to hormonal imbalances. - Common Nutritional Pitfalls:
- Skipping meals, leading to blood sugar imbalances
- Over-reliance on processed, prepackaged foods
- Inadequate fiber intake, impairing estrogen detoxification
- What You Can Do:
- Focus on balanced, nutrient-dense meals with a mix of lean proteins, healthy fats, and complex carbohydrates.
- Add more anti-inflammatory foods to your diet, such as leafy greens, berries, nuts, seeds, and olive oil.
- Ensure sufficient intake of vitamin D (from sunlight or supplements) and magnesium (found in almonds, spinach, and dark chocolate).
- Stay hydrated to support overall health and digestive function.
5. Ignoring or Delaying Medical Care
Delays in diagnosis and treatment are common in endometriosis, but ignoring symptoms or putting off care can worsen the condition. Without proper management, endometriosis can lead to complications like severe pain, infertility, and organ damage. For some women, the damage can results in the removal of their uterus, ovaries, and sometimes parts of other organs such as sections of the intestines.
- Why it Worsens Endometriosis:
Endometriosis lesions can grow and spread over time, causing more inflammation and scarring. Pain can become chronic and harder to treat if left unaddressed. Lack of medical care may also mean missing out on effective treatments like hormonal therapies, surgery, or lifestyle interventions. - What You Can Do:
- Advocate for yourself by seeking a gynecologist or specialist experienced in endometriosis.
- Keep a detailed symptom diary to share with your healthcare provider, including pain levels, cycle patterns, and triggers.
- Explore a multidisciplinary approach, combining conventional treatments (e.g., laparoscopic surgery, hormonal therapies) with lifestyle changes and complementary therapies like acupuncture or pelvic floor physical therapy.
- Stay informed about new developments in endometriosis care, such as advancements in non-invasive diagnostic tools or new treatment options.
Conclusion
Managing endometriosis effectively requires an understanding of what can worsen symptoms and taking proactive steps to address those factors. Chronic inflammation, hormonal imbalances, high stress levels, poor nutrition, and delays in medical care can all exacerbate the condition, but they can be mitigated through lifestyle adjustments, a supportive healthcare team, and self-advocacy. Building a strong support system of healthcare providers, loved ones, and others who understand the challenges of endometriosis can make a significant difference. Additionally, staying informed about treatment options and new research empowers individuals to make choices that align with their needs. Each person’s journey with endometriosis is unique, so finding what works for your body and prioritizing your well-being are essential steps toward living a more comfortable and empowered life.