Addressing Uterine Health Disparities
Why Women of Color Face Greater Challenges and How We Can Close the Gap
Why We Must Address Uterine Health Disparities in Women of Color
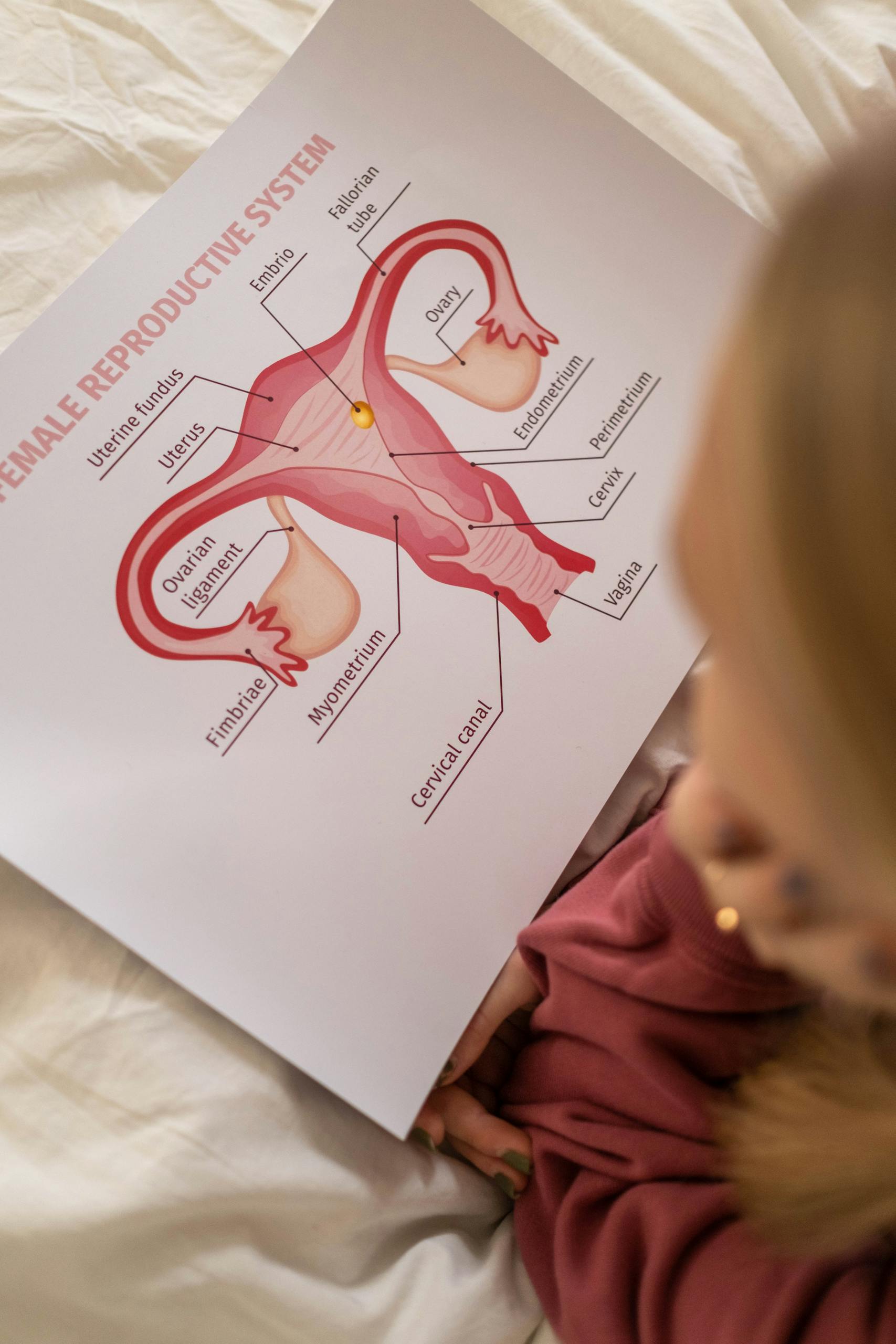
Health disparities remain a pervasive issue across the healthcare landscape, with profound impacts on the well-being of underserved and marginalized populations. Among these, uterine-related health disparities in women of color stand out as a significant yet often overlooked concern. Conditions such as uterine fibroids, endometriosis, and adenomyosis disproportionately affect Black, Hispanic, and Indigenous women. These disparities are not merely medical but are also rooted in systemic inequities, cultural stigmas, and historical neglect. This makes them a pressing public health issue.
This article delves into the multiple dimensions of uterine-related health disparities in women of color. This article highlights the urgency of addressing these inequalities, exploring their underlying causes, and proposing pathways for change.
1. Disproportionate Prevalence of Uterine Conditions
Higher Rates of Uterine Fibroids
Uterine fibroids are benign growths in the uterus, yet their impact on quality of life can be severe. For example, studies indicate that up to 80% of Black women will develop fibroids by the age of 50, compared to around 70% of white women. Not only are fibroids more common in Black women, but they also tend to develop earlier, grow larger, and cause more severe symptoms, including heavy menstrual bleeding, pelvic pain, and fertility issues.
Endometriosis and Misdiagnosis
Endometriosis, another common uterine-related condition, involves the growth of uterine-like tissue outside the uterus. Although historically underdiagnosed in Black and Hispanic women, emerging research shows that women of color are just as likely, if not more likely, to develop endometriosis as their white counterparts. The myth that endometriosis predominantly affects affluent white women has contributed to delayed diagnoses in women of color. This not only exacerbates symptoms but also limits their treatment options.
Adenomyosis
Adenomyosis, a condition where the uterine lining grows into the uterine muscle, also disproportionately impacts women of color. Symptoms like heavy, prolonged periods and severe pelvic pain are often dismissed or normalized, leading to delays in diagnosis and management.
2. Delayed Diagnoses and Mismanagement
Systemic Bias in Healthcare
Implicit biases in the healthcare system frequently result in the dismissal of pain and other symptoms reported by women of color. Black women are often perceived as having a higher pain tolerance, a stereotype rooted in racial prejudice. As a result, they are less likely to receive adequate pain management or timely diagnostic interventions.
Normalization of Symptoms
Cultural and societal narratives often normalize severe menstrual pain or heavy bleeding, leading women to tolerate symptoms rather than seek medical care. In many communities of color, such symptoms are regarded as “just a part of being a woman,” delaying the recognition of conditions like fibroids or adenomyosis as abnormal.
3. Barriers to Accessing Care
Economic Inequities
Economic disparities significantly impact access to healthcare for women of color. Black and Hispanic women are more likely to be uninsured or underinsured, limiting their ability to afford diagnostic tests, treatments, or specialist consultations.
Geographical Disparities
Women of color in rural areas often face limited access to gynecologists or reproductive health specialists. This geographical barrier delays the diagnosis and treatment of uterine-related conditions, further exacerbating disparities.
Cultural and Linguistic Barriers
Language barriers and cultural differences can also hinder access to care. For instance, Hispanic women with limited English proficiency may struggle to communicate their symptoms effectively or may feel less comfortable advocating for themselves in healthcare settings.
4. Inequitable Treatment Options
Overuse of Hysterectomies
Black women, are more likely to undergo hysterectomies for conditions like fibroids, often without being offered less invasive alternatives (such as uterine artery embolization or myomectomy). This reflects both a lack of access to advanced treatment options and a failure to adequately inform patients about their choices.
Underutilization of Fertility-Preserving Treatments
For women of color who wish to preserve fertility, options like minimally invasive surgery or hormonal treatments may not be presented due to biases or assumptions about their reproductive desires. This inequity has profound implications for their ability to plan families on their terms.
5. Consequences for Maternal Health
Complications During Pregnancy
Uterine conditions such as fibroids and endometriosis can increase the risk of pregnancy complications, including preterm birth, placental abruption, and miscarriage. Black women already face a threefold higher risk of maternal mortality compared to white women, and untreated uterine conditions further heighten this risk.
Impact on Fertility
Untreated uterine conditions can lead to infertility, a devastating consequence for many women. Women of color are often referred to fertility specialists later than their white counterparts, reducing their chances of successful outcomes.
6. Cultural and Societal Stigmas
Silence Around Reproductive Health
In many communities of color, discussions about reproductive health are stigmatized or considered taboo. This silence prevents women from seeking care or sharing their experiences, perpetuating a cycle of suffering and neglect.
Distrust in Healthcare
Historical injustices, such as forced sterilizations of Black and Indigenous women, have created a deep-seated mistrust of the medical system. This distrust can discourage women from seeking care or following through with recommended treatments.
7. Lack of Representation in Research
Underrepresentation in Clinical Trials
Women of color are often excluded from clinical trials studying uterine-related conditions. This exclusion results in a lack of understanding about how these conditions present and progress in diverse populations, leading to gaps in evidence-based care.
Need for Culturally Competent Research
Research that considers cultural, genetic, and environmental factors is crucial for developing effective treatments and interventions. Without this focus, healthcare providers may rely on data that do not reflect the needs of women of color.
8. Pathways to Change
Cultural Competency Training for Providers
Healthcare providers must undergo training to recognize and address their implicit biases, communicate effectively with diverse populations, and provide culturally sensitive care.
Community Outreach and Education
Empowering women of color with knowledge about uterine health can help them recognize symptoms, seek care early, and advocate for themselves. Community-based programs can play a pivotal role in breaking down stigmas and providing resources.
Policy Changes and Advocacy
Policymakers must address systemic barriers by expanding healthcare access, funding research on health disparities, and incentivizing providers to offer equitable, patient-centered care.
Representation in Medicine
Increasing the representation of women of color in medical and research fields can help ensure that their voices and experiences are included in shaping healthcare policies and practices.
9. Empowering Women of Color
At the heart of addressing uterine-related health disparities is the need to empower women of color to take charge of their reproductive health. This involves not only improving access to care but also fostering a culture where their concerns are heard, validated, and acted upon.
Conclusion
Uterine health disparities in women of color are a reflection of broader systemic inequities in healthcare. These disparities affect not only individual health outcomes but also families, communities, and society as a whole. By shining a light on these issues, advocating for equitable care, and fostering awareness, we can take meaningful steps toward closing the gap and ensuring that all women receive the care they deserve.
This is not just a medical issue—it is a matter of social justice, equity, and humanity. Addressing uterine health disparities requires the collective efforts of healthcare providers, researchers, policymakers, and communities to build a future where every woman, regardless of her background, can thrive in health and well-being.