Adenomyosis vs Endometriosis
Key Differences, Similarities, and Impacts
Adenomyosis vs endometriosis are two gynecological conditions that are often discussed together due to their overlapping symptoms and impact on reproductive health. However, they are distinct entities with unique pathophysiological mechanisms, clinical manifestations, and management strategies. This articles provides a comprehensive overview of the differences and similarities between adenomyosis vs endometriosis.
Definition and Pathophysiology
Adenomyosis
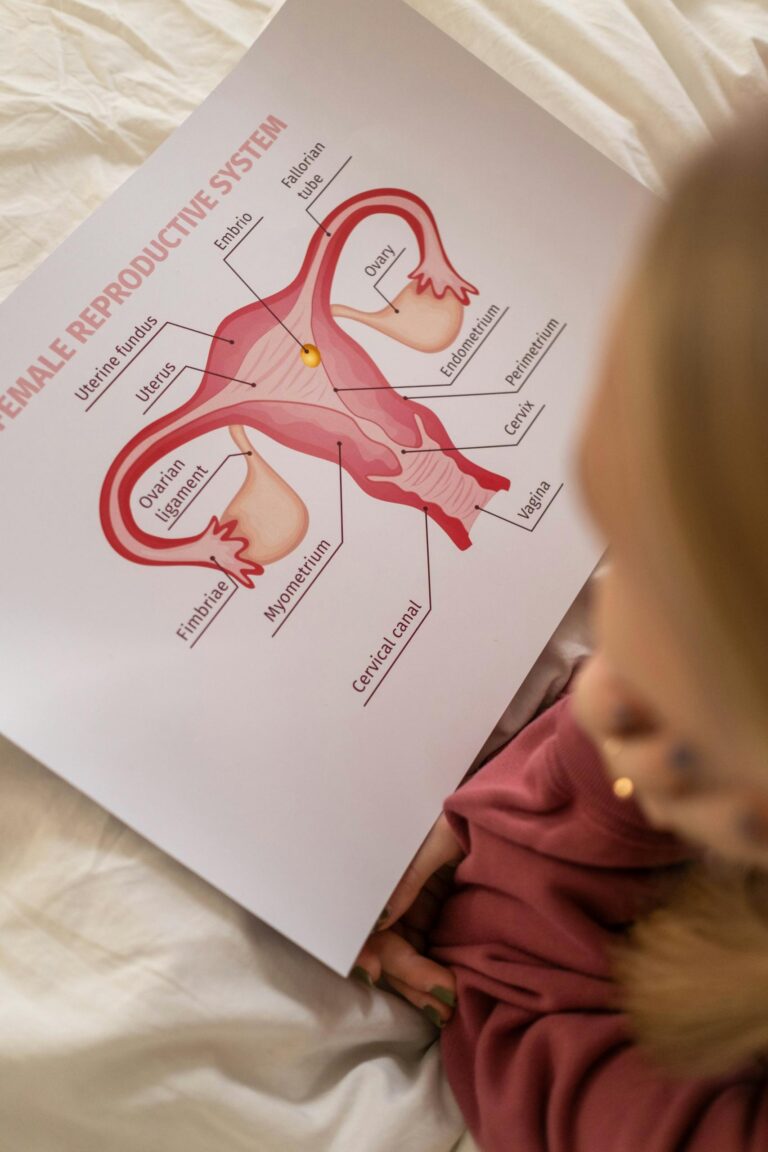
Adenomyosis is a condition characterized by the presence of endometrial tissue (glands and stroma) within the myometrium, the muscular layer of the uterus. This ectopic endometrial tissue induces hypertrophy and hyperplasia of the surrounding myometrium, leading to a diffusely enlarged uterus.
- Pathogenesis: The exact cause of adenomyosis is unclear, but several theories exist, including:
- Invagination Theory: Endometrial tissue invaginates into the myometrium through weakened areas of the uterine wall.
- De Novo Development: Endometrial tissue arises from pluripotent stem cells within the myometrium.
- Inflammation and Hormonal Factors: Chronic inflammation and elevated levels of estrogen may contribute to disease progression.
Endometriosis
Endometriosis is a condition where endometrial-like tissue grows outside the uterus, commonly on the ovaries, fallopian tubes, pelvic peritoneum, and other distant sites such as the diaphragm or lungs.
- Pathogenesis: The cause of endometriosis is also not fully understood, but several theories include:
- Retrograde Menstruation: Menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity.
- Coelomic Metaplasia: Transformation of peritoneal cells into endometrial-like cells under hormonal or environmental influences.
- Immune Dysregulation: Defective immune responses fail to clear ectopic endometrial cells.
Epidemiology
Adenomyosis
- Prevalence: Common in women aged 35-50 years, particularly those with a history of multiple pregnancies.
- Risk Factors:
- Multiparity (having given birth multiple times)
- Uterine surgeries, such as cesarean sections or fibroid removal
- Estrogen dominance
Endometriosis
- Prevalence: Affects approximately 10% of women of reproductive age.
- Risk Factors:
- Early menarche and short menstrual cycles
- Family history of endometriosis
- Nulliparity (not having given birth)
- High estrogen levels
Symptoms
Adenomyosis
- Menstrual Symptoms:
- Heavy menstrual bleeding (menorrhagia)
- Painful periods (dysmenorrhea), often worsening over time
- Pelvic Symptoms:
- Chronic pelvic pain
- Uterine tenderness or an enlarged uterus palpable during a pelvic exam
- Reproductive Symptoms:
- Subfertility or infertility (less common compared to endometriosis)
Endometriosis
- Menstrual Symptoms:
- Painful periods (dysmenorrhea), often severe
- Pelvic Symptoms:
- Chronic pelvic pain
- Pain during intercourse (dyspareunia)
- Pain during bowel movements or urination, especially during menstruation
- Reproductive Symptoms:
- Infertility or difficulty conceiving, a hallmark of the condition
Pathological Features
Adenomyosis
- Gross Appearance: Diffusely enlarged uterus with thickened myometrium, often described as “boggy.”
- Microscopic Features: Presence of endometrial glands and stroma within the myometrium, surrounded by smooth muscle hyperplasia.
Endometriosis
- Gross Appearance: Lesions ranging from superficial implants on the peritoneum to deep infiltrating nodules; chocolate cysts (endometriomas) on the ovaries.
- Microscopic Features: Endometrial-like glands, stroma, and associated inflammatory response; fibrotic changes in chronic cases.
Diagnosis
Adenomyosis
- Imaging:
- Ultrasound: Thickened junctional zone and heterogenous myometrium.
- MRI: High sensitivity for detecting adenomyosis, showing an enlarged junctional zone (>12 mm).
- Definitive Diagnosis: Requires histopathological examination after hysterectomy.
Endometriosis
- Imaging:
- Ultrasound: Useful for identifying endometriomas but less effective for superficial peritoneal lesions.
- MRI: Can detect deep infiltrating endometriosis.
- Laparoscopy: Gold standard for diagnosis, allowing direct visualization and biopsy of lesions.
Treatment Options
Adenomyosis
- Medical Management:
- Hormonal therapies, such as oral contraceptives, progestins, or gonadotropin-releasing hormone (GnRH) agonists/antagonists.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief.
- Surgical Management:
- Hysterectomy is the definitive treatment for women who have completed childbearing.
- Uterine-sparing procedures, such as adenomyomectomy, for women desiring fertility.
Endometriosis
- Medical Management:
- Hormonal therapies, including oral contraceptives, progestins, or GnRH agonists/antagonists.
- NSAIDs for symptom control.
- Surgical Management:
- Laparoscopic excision or ablation of endometriotic lesions.
- Removal of endometriomas or other affected structures.
- Hysterectomy with or without oophorectomy for severe, refractory cases.
- Fertility Treatment:
- Assisted reproductive technologies (ART), such as in-vitro fertilization (IVF), for women with infertility.
Impact on Fertility
Adenomyosis
- Adenomyosis may impair fertility by disrupting normal uterine contractility, implantation, and vascularization. However, its impact is generally less pronounced than that of endometriosis.
Endometriosis
- Endometriosis significantly affects fertility by causing adhesions, distorting pelvic anatomy, and impairing egg quality or ovulation. Approximately 30-50% of women with endometriosis experience infertility.
Similarities
- Hormonal Dependence: Both conditions are estrogen-dependent and often improve after menopause.
- Chronic Pain: Both cause significant pelvic pain that can affect quality of life.
- Overlap in Symptoms: Dysmenorrhea, menorrhagia, and chronic pelvic pain are common in both conditions.
- Association with Infertility: Both conditions can contribute to difficulties in conceiving, albeit to varying extents.
- Diagnostic Challenges: Both are under-diagnosed and often require advanced imaging or surgical confirmation.
Key Differences
| Feature | Adenomyosis | Endometriosis |
|---|---|---|
| Location | Endometrial tissue within the myometrium | Endometrial-like tissue outside the uterus |
| Age Group | Common in women >35 years | Common in women of reproductive age |
| Uterus Size | Enlarged, often boggy | Normal-sized uterus |
| Infertility Impact | Less common but possible | Affects 30-50% of patients |
| Definitive Diagnosis | Histopathology post-hysterectomy | Laparoscopy with biopsy |