Introduction to Endometriosis
What is Endometriosis?
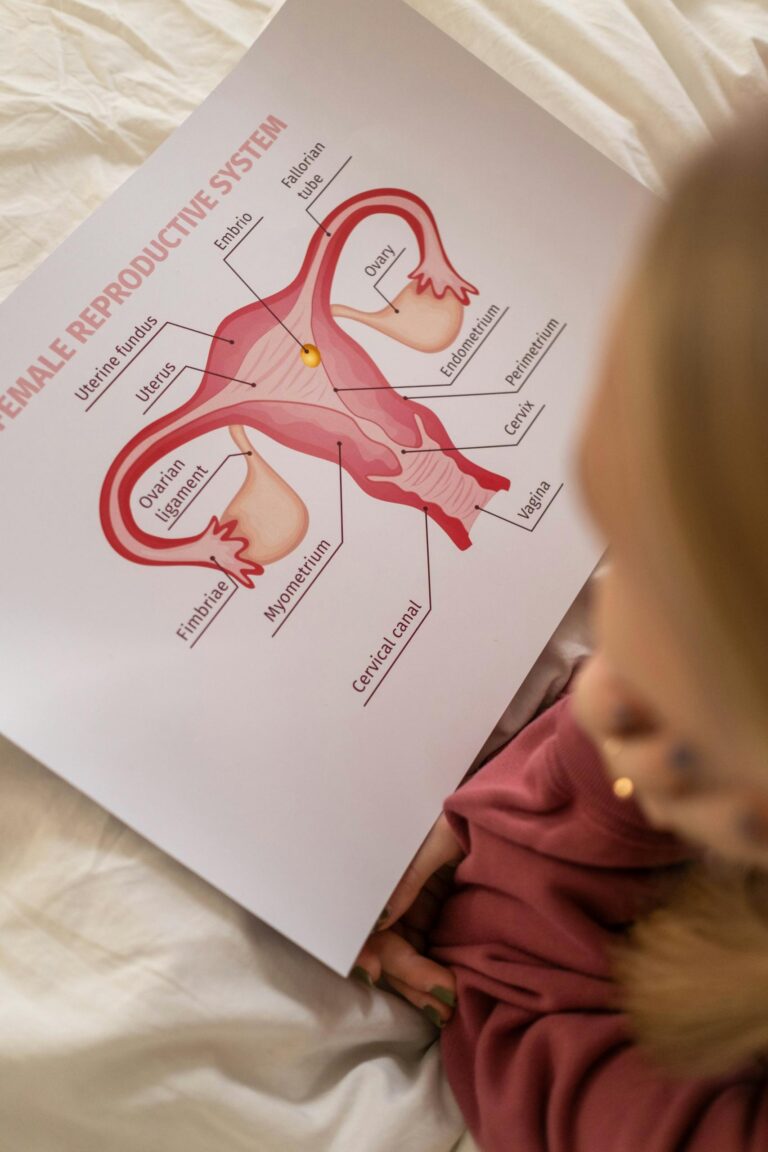
Endometriosis is a chronic condition where tissue similar to the uterine lining (endometrium) grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining. Sometimes the tissue can spread to the diaphragm, lungs (thoracic endometriosis), brain (rare), surgical scars, bladder, or intestines.
This tissue responds to hormonal changes, leading to inflammation, pain, and sometimes scar tissue. It can affect fertility and overall quality of life.
Endometriosis affects about 10% of women of reproductive age globally, approximately 190 million people. Many remain undiagnosed—studies suggest delays in diagnosis average 7–10 years, with an estimated 50–60% of cases undetected due to misdiagnosis or asymptomatic presentations.
What Causes Endometriosis?
The exact cause is still unknown. However, possible factors include:
- Retrograde menstruation: Menstrual blood flows backward into the pelvic cavity instead of exiting the body.
- Genetics: Family history increases risk.
- Immune dysfunction: The body fails to clear abnormal tissue.
- Metaplasia: Normal cells transform into endometrial-like tissue.
- Hormonal factors: Excessive estrogen may promotes its growth.
What are Common Signs and Symptoms?
- Pelvic pain (especially with periods)
- Pain during intercourse or bowel movements
- Heavy or irregular periods
- Infertility
- Fatigue, bloating, or nausea
Less Common Signs and Symptoms Include:
- Chest pain or coughing blood (thoracic endometriosis)
- Sciatic nerve pain
- Blood in stool or urine
- Infertility without pain
Diagnosis
An official diagnosis of endometriosis typically requires:
- Symptom Review: Detailed discussion of pain, menstrual history, and other signs.
- Imaging Tests: Ultrasound or MRI to identify cysts or lesions (not definitive yet).
- Laparoscopy: A minimally invasive surgery to visually inspect and biopsy lesions—this is the gold standard for diagnosis.
Treatment
Treatment for endometriosis depends on the severity of symptoms, the individual’s age, and whether they want to preserve fertility. The main goals are to reduce pain, manage symptoms, and improve fertility outcomes when necessary. Treatment options include:
Medications:
- Pain Relief: Over-the-counter pain relievers like ibuprofen or naproxen.
- Hormonal Therapy:
- Birth Control Pills: Helps suppress menstrual cycles and reduce symptoms by overriding the body’s natural estrogen levels.
- Progestins: Can suppress menstruation and shrink endometrial tissue.
- GnRH Agonists: Induce a temporary menopause-like state by suppressing estrogen production, which shrinks endometrial growths.
- IUDs: Hormonal intrauterine devices (IUDs) can reduce menstrual flow and ease pain.
- Aromatase Inhibitors: Block estrogen production in the body, sometimes used alongside GnRH agonists for added effect.
- Danazol: A synthetic steroid that suppresses the production of estrogen, but has significant side effects.
Surgery:
- Laparoscopic Surgery: The gold standard for removing endometrial tissue, especially for those who have severe pain or want to preserve fertility.
- Hysterectomy: In cases where other treatments fail, removing the uterus and sometimes the ovaries may be recommended.
Lifestyle Changes and Complementary Therapies:
- Dietary Changes: Anti-inflammatory diets or avoiding foods that can increase estrogen may help manage symptoms.
- Physical Therapy: Pelvic floor therapy can help reduce pain and improve mobility.
- Alternative Therapies: Acupuncture and herbal treatments are sometimes used to reduce pain, though their effectiveness varies.
The treatment plan is personalized, and in some cases, a combination of approaches is used.
Risk Factors
Several factors can increase the risk of developing endometriosis. The most common risk factors include:
1. Family History:
- Having a mother or sister with endometriosis increases the likelihood of developing the condition, suggesting a potential genetic link.
2. Age:
- Endometriosis most commonly affects women in their 30s and 40s, but it can occur at any age, even in teenagers.
3. Menstrual History:
- Early onset of menstruation (before age 11)
- Longer menstrual cycles (more than 27 days)
- Heavy or prolonged periods (lasting more than 7 days)
4. Nulliparity (No Pregnancy):
- Women who have never been pregnant are at higher risk, possibly because pregnancy can reduce the menstrual flow and the growth of endometrial tissue.
5. Immune System Issues:
- Women with immune system disorders, like autoimmune diseases, may be more susceptible, possibly due to an immune response that doesn’t clear displaced endometrial tissue effectively.
6. Structural Abnormalities:
- Conditions like a narrow cervix or abnormal uterus shape can prevent menstrual blood from flowing normally, potentially leading to retrograde menstruation, which may increase the risk of developing endometriosis.
7. Exposure to Environmental Toxins:
- Certain environmental chemicals and toxins, such as dioxins (found in some pesticides and industrial processes), may contribute to the development of endometriosis, though the evidence is not yet conclusive.
8. Estrogen Exposure:
- High levels of estrogen may promote the growth of endometriosis. This can be influenced by lifestyle factors such as obesity (which increases estrogen production) or prolonged exposure to estrogen through hormonal therapies.
9. Ethnicity:
- Some studies suggest that Caucasian women may have a slightly higher risk of developing endometriosis compared to women from other ethnic groups, though endometriosis can affect women of all ethnicities and this finding may be explained by this resource.
These risk factors are not definitive causes but may contribute to the likelihood of developing endometriosis.
What Can Exacerbate Endometriosis?
Several factors can exacerbate the symptoms of endometriosis or make the condition worse. These include:
1. High Estrogen Levels:
- Hormonal Fluctuations: Estrogen promotes the growth of endometrial tissue. High estrogen levels, whether from natural hormonal cycles or external sources (like birth control pills, hormone replacement therapy, or obesity), can worsen symptoms.
2. Diet and Inflammation:
- Pro-inflammatory Foods: Diets high in processed foods, sugar, trans fats, and red meat can increase inflammation, which may aggravate endometriosis symptoms.
- Low Omega-3 Fatty Acids: Diets low in anti-inflammatory omega-3 fatty acids (found in fish, flaxseeds, etc.) may make symptoms worse.
3. Stress:
- Chronic Stress: Stress can lead to hormonal imbalances, including increased estrogen production, which may exacerbate symptoms like pain and inflammation. It can also increase muscle tension in the pelvic region, leading to more discomfort.
4. Lack of Exercise or Sedentary Lifestyle:
- Physical Inactivity: Regular exercise can help reduce inflammation, improve hormone balance, and relieve pain. A sedentary lifestyle may worsen pain and increase stress levels, both of which can exacerbate endometriosis.
5. Smoking:
- Nicotine and Toxins: Smoking has been linked to a higher risk of developing endometriosis and can worsen symptoms. Nicotine and other chemicals in cigarettes may also impact hormonal balance and immune function, promoting endometrial growth.
6. Exposure to Environmental Toxins:
- Endocrine Disruptors: Chemicals such as dioxins, PCBs (polychlorinated biphenyls), and phthalates, which can be found in some plastics, pesticides, and industrial products, have been shown to interfere with hormone regulation and may exacerbate endometriosis.
7. Not Managing Pain Early:
- Delayed Treatment: Ignoring or not addressing pain symptoms early on can lead to worsening of the disease, as untreated endometriosis may lead to scar tissue (adhesions) and further complications like infertility.
8. Menstrual Irregularities:
- Heavy Periods and Retrograde Menstruation: If menstrual blood flows backward into the pelvic cavity (retrograde menstruation), it can worsen endometriosis by spreading endometrial cells outside the uterus.
9. Lack of Sleep:
- Sleep Deprivation: Poor sleep can increase stress and inflammation, potentially exacerbating endometriosis symptoms. Proper rest is essential for overall hormone regulation and pain management.
10. Certain Medications:
- Medications that Affect Hormones: Certain medications, especially those that increase estrogen levels (e.g., some types of hormone replacement therapy), may worsen symptoms.
Managing these factors through lifestyle changes, medication, or dietary adjustments can help reduce the exacerbating effects on endometriosis.
If left untreated, endometriosis can lead to a variety of physical, emotional, and reproductive consequences, including:
Chronic Pain:
- Pelvic Pain: One of the most common and debilitating symptoms, which may become more severe over time if untreated. This pain may include severe menstrual cramps, pain during intercourse, bowel movements, or urination.
- Painful Adhesions: Endometriosis can lead to the formation of scar tissue (adhesions), which can cause organs to stick together, resulting in severe pain.
Infertility:
- Reproductive Challenges: Endometriosis is a leading cause of infertility. The condition can affect the ovaries, fallopian tubes, and uterus, making it harder for an egg to be fertilized or implanted. It’s estimated that 30–50% of women with endometriosis may struggle with fertility.
Ovarian Cysts (Endometriomas):
- Endometriomas (Chocolate Cysts): These cysts form on the ovaries and can lead to long-term damage, including reduced ovarian function, which could impact fertility.
- Ovary Damage: If untreated, endometriosis can lead to permanent damage or scarring of the ovaries, further compromising fertility.
Increased Risk of Other Health Conditions:
- Chronic Inflammation: Endometriosis causes chronic inflammation, which, if left unchecked, could potentially contribute to other health issues such as autoimmune disorders or increased risk of certain cancers, including ovarian cancer.
- Bowel and Urinary Problems: Endometriosis can involve the bowel or urinary tract, leading to pain, discomfort, and potential complications like bowel obstruction or urinary tract infections.
Emotional and Mental Health Strain:
- Depression and Anxiety: Chronic pain, fertility struggles, and the impact on daily life can lead to depression, anxiety, and other mental health issues. The emotional toll can be significant, especially if symptoms are severe and disrupt normal functioning.
- Decreased Quality of Life: Endometriosis can significantly affect a person’s quality of life, limiting daily activities, work productivity, and social interactions.
Progression of Disease:
- Worsening Symptoms: Without treatment, the endometrial tissue may continue to grow, leading to more severe symptoms. This can cause worsening pain, the spread of endometrial implants, and more extensive tissue damage.
- Organ Involvement: In advanced cases, untreated endometriosis can affect other organs, such as the bladder, intestines, and kidneys, leading to more severe complications and requiring more invasive treatments.
Adhesions and Organ Damage:
- Scarring and Adhesions: The endometrial tissue can cause scarring, or adhesions, which may lead to organs sticking together. This can result in pain, digestive issues, or difficulty in surgical interventions.
Risk to Overall Reproductive Health:
- Increased Risk of Ectopic Pregnancy: Women with untreated endometriosis may have an increased risk of ectopic pregnancies, where the embryo implants outside the uterus, which can be life-threatening if not treated promptly. Ectopic pregnancies are not viable and will always result in a miscarriage.
Hysterectomy in Severe Cases:
- Hysterectomy as a Last Resort: In cases where other treatments have failed and the individual no longer wishes to conceive, a hysterectomy (removal of the uterus) may be recommended to alleviate pain and other symptoms. However, this is typically considered only after other options have been explored.
Leaving endometriosis untreated can have serious long-term effects, so early diagnosis and intervention are important for managing symptoms, preserving fertility, and improving quality of life.
Conclusion
In conclusion, you’ve learned that endometriosis is a chronic condition where tissue similar to the uterine lining grows outside the uterus, causing pain, inflammation, and potential fertility issues. The exact cause is unknown, but factors such as hormonal imbalances, genetics, and immune dysfunction may play a role. Common symptoms include pelvic pain, painful menstruation, and infertility, while less common symptoms can involve chest pain or blood in the stool.
Endometriosis is diagnosed through symptom assessment, imaging tests, and the gold-standard laparoscopy. Treatment options range from medications (pain relievers, hormonal therapies) to surgery (laparoscopy or hysterectomy), and lifestyle changes like diet and exercise may help manage symptoms.
Risk factors include family history, early menstruation, and estrogen exposure, while certain factors like stress, smoking, and inflammatory foods can exacerbate the condition. Left untreated, endometriosis can lead to chronic pain, infertility, and severe organ damage, making early diagnosis and intervention crucial for improving outcomes and quality of life.